You may have heard of Polycystic Ovary Syndrome (PCOS), or you may be living with the condition and not even know it. PCOS is a complicated condition and one that many women have to live with.
This blog is all about what PCOS is and what causes it, the symptoms associated with this condition, and ways to manage it so you can live your life without disruption.
Indeed, with the right knowledge, you can take control of your health and understand exactly what you need to do. So, let’s start by learning more about Polycystic Ovary Syndrome (PCOS).
Introduction to Polycystic Ovary Syndrome (PCOS)
Are you experiencing irregular periods, hair growth in unwanted places, or infertility issues?
If so, it may be time for you to learn about PCOS!
PCOS is a hormonal disorder that affects women of reproductive age. It’s caused by an imbalance in the hormones that regulate our menstrual cycles. This hormone imbalance can lead to a variety of symptoms, including irregular periods and infertility, weight gain, acne, and excess hair growth in unwanted places like your face and chest. It can also cause emotional issues like depression and anxiety.
If left untreated, PCOS can have long-term health consequences, like type 2 diabetes and heart disease. On the plus side, many treatments are available that can help manage the effects and improve your quality of life.
What are the Causes of PCOS?
PCOS or Polycystic Ovary Syndrome is a set of hormonal imbalances and metabolic changes affecting millions of women worldwide.
But why do they occur in the first place? Well, the exact cause of PCOS is still unknown—though some experts believe it results from a combination of genetics, environmental factors, and lifestyle choices.
Family history is a major factor that can contribute to developing PCOS. Women with mothers or sisters who have the syndrome are more likely to develop it themselves. The same goes for medical conditions like insulin resistance or obesity—if someone in your family has them, then you may be at a higher risk for having PCOS.
Lifestyle factors such as diet and exercise choices have also been linked to developing PCOS. A poor diet high in sugar and processed foods can lead to weight gain, which has been associated with an increased risk for the condition. And lack of exercise can also increase your odds of having the syndrome.
Ultimately, we’re still learning more about what causes PCOS—but it’s clear that several genetic and environmental factors likely play a role in its development.
What are the Symptoms of PCOS?
If you’ve been diagnosed with PCOS, you’re likely wondering what symptoms it may cause. PCOS can cause a wide range of physical and emotional symptoms. The severity of these symptoms can vary based on each individual. Some common signs of PCOS are:
- Irregular periods — this could mean skipping periods, having fewer than usual, or having very heavy periods. While you can manage heavy bleeding with the help of best sanitary pads for heavy flow, it’s not a good sign.
- Excessive hair growth, or hirsutism — this includes thick, dark hairs in places like the chin, chest, and abdomen
- Acne — often in the form of cysts or blemishes
- Skin discoloration — often patches of dark skin on the neck or body folds
- Weight gain or difficulty losing weight
- Thinning hair on the scalp
- Fertility issues — difficulties getting pregnant due to ovulation problems
- Anxiety or depression due to hormonal imbalances which can affect mood and energy levels
The good news is that there are treatments available for PCOS. Once a correct diagnosis is established, talk to your doctor about methods that can help reduce your symptoms and improve your overall health.
Diagnosis and Tests for PCOS
The diagnosis and tests for PCOS can vary depending on the symptoms present in each individual. Generally, the process will involve a physical exam, blood tests to measure hormones, and an ultrasound of the ovaries.
-
Physical Exam
During a physical exam, your doctor will examine your body to look for signs of PCOS such as excess hair growth, acne, or skin discoloration. Your medical history, menstrual cycle history, and any existing symptoms will also be taken into account during the physical exam.
-
Blood Tests
Your doctor may order blood tests to measure hormone levels. These include testosterone and luteinizing hormone (LH), which are generally higher among women with PCOS. Other more specific hormones that may be tested include follicle-stimulating hormone (FSH), prolactin, and 17-alpha hydroxyprogesterone (17-OHP).
-
Ultrasound
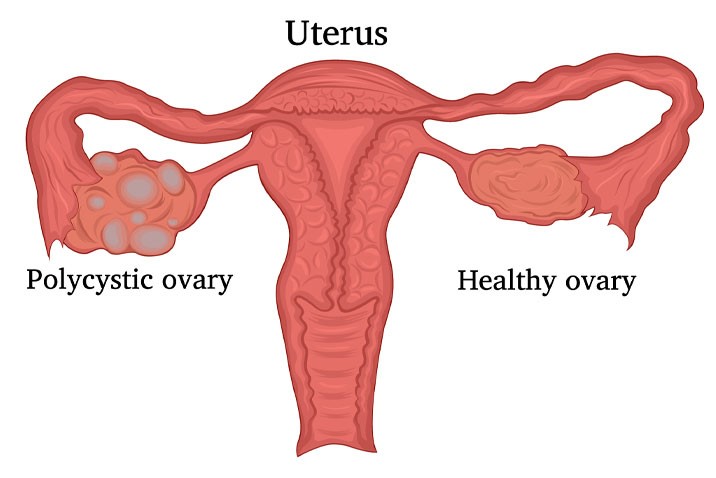
An ultrasound of the ovaries is frequently used to diagnose PCOS as it can show whether or not small cysts are present in the ovaries. The ultrasound can also help determine whether there is an increased amount of follicles in each ovary – another indicator of PCOS.
Management and Treatment of PCOS
PCOS is, fortunately, a manageable condition and there are many treatments available for managing its symptoms. Depending on your symptoms, your doctor or healthcare professional may prescribe a variety of medications to help reduce androgen levels, induce ovulation, or reduce the risk of diabetes.
1. Diet
One of the easiest and most effective ways to manage PCOS is to make dietary changes. A balanced diet low in sugar, refined carbohydrates, and saturated fats can help keep your body weight within a healthy range and also balance your insulin levels. Eating plenty of fiber-rich foods and avoiding processed foods can also help improve your body’s response to insulin and promote regular ovulation.
2. Exercise
Exercise is beneficial in the management of PCOS—it helps regulate hormones and reduce insulin resistance by increasing insulin sensitivity, which ultimately improves the chances of ovulation. Aiming for at least 30 minutes of moderate physical activity five days per week is recommended for most people with PCOS.
3. Supplements
There are some supplements you can take to help manage PCOS symptoms as well. Vitamin D helps reduce testosterone levels in some women with PCOS, and omega-3 fish oil supplements have been linked with improved fertility rates in women with polycystic ovary syndrome.
Additionally, increasing intake of anti-inflammatory nutrients like zinc, chromium polynicotinate, vitamin C, selenium, alpha lipoic acid (ALA), folate (B9), magnesium, and calcium citrate has been connected to reduced inflammation and improved fertility outcomes as well.
Hence, PCOS is a complex but treatable chronic condition. Although there is no single cause or cure, there are a few lifestyle changes and medical treatments that can help you manage PCOS and its symptoms.
However, eating a balanced diet, exercising regularly, and getting enough rest are key to managing PCOS. Additionally, medication such as Metformin or hormone therapy can help regulate hormones and minimize symptoms.
If you think you may have PCOS, it’s important to talk to a healthcare practitioner and get tested. Indeed, with the right knowledge and the right treatment plan, managing PCOS is possible.